Fast Facts
Stop aspirin and other medications causing bleeding one week before surgery.
If you notice swelling in the wound or trouble breathing after surgery tell the nurse immediately.
There’s a small risk of permanent change in voice.
Take two weeks off to recover.
What is this for? Is it effective?
Parathyroidectomy means removing one or more of the parathyroid glands.
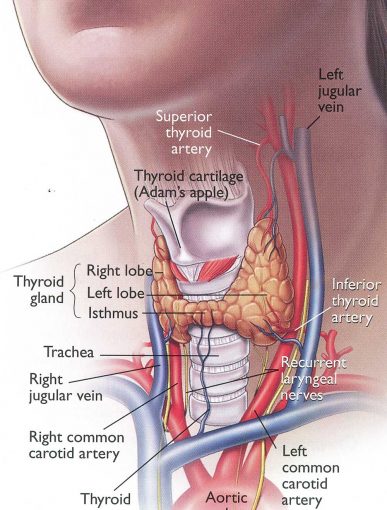
There are 4 parathyroid glands, two on each side of the neck, close to the thyroid gland and trachea/windpipe. They are small, around 5x7mm each.
Parathyroid glands make parathyroid hormone (PTH). This hormone is essential for short and long term calcium balance in the blood and bones. A normal level of calcium is necessary for nerves, the heart, the gut, the kidneys and bones to function normally. A high PTH level can cause a high calcium level, affecting kidney function and bone strength and causing fatigue and aches/pains. A low PTH level can cause a low calcium level, causing pins and needles sensation, muscle cramps/spasms, irregular heart beat and seizures.
The parathyroid gland or glands may need to be removed if they become overactive, making too much PTH and causing high calcium levels. This can be due to a single overactive gland (parathyroid adenoma or tumour) or all glands being overactive (4 gland hypertrophy). Parathyroid adenoma/tumour are almost always benign.
Tests for parathyroid disease:
- Blood test for PTH, calcium and kidney function
- Ultrasound shows the size and shape of the thyroid gland. Healthy parathyroid glands are usually too small to be seen on ultrasound. A large or overactive parathyroid gland may be picked up on ultrasound.
- Sestamibi scan can detect an overactive parathyroid gland
- 4D CT of the neck and chest can detect the precise location of an overactive gland.
- DEXA scan to look for bone health (osteopenia and osteoporosis).
Surgery to remove a single parathyroid adenoma has a very high rate of permanent cure. Surgery for 4 gland hypertrophy is more challenging and 1:10 people may need more surgery if the PTH level remains high.
